Presentation to respiratory physician:
-
•22 year old man still working as a farmer
-
•Recurrent chest infections – Pulmicort (budesonide/steroid) and Salbutamol inhalers.

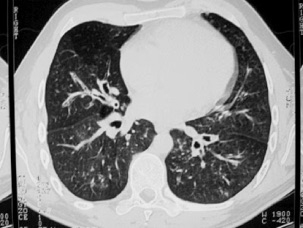
•surgical clips in region of lower oesophagus
•prominence and dilatation of the bronchi centrally in generalised pattern throughout the lungs
•no definite ground glass appearance
•no subpleural lines
•volume loss in right upper zone
•widespread bronchiectatic change
•no focal area of severe change
•FEV1 2.11 50% predicted
•FVC 2.70 54% predicted
Reason for referral to Thoracic Surgeon:
•Referred by Respiratory Physician with diagnosis of BRONCHIECTASIS.
•Is there a place for lung resection?
Review of symptoms:
•Coughs immediately after swallowing anything – liquids worse than solids.
•Recurrent chest infections – Pulmicort (budesonide/steroid) and Salbutamol inhalers.
•Dysphagia for solids.
•Intermittent epigastric discomfort (tight) – unaffected by Sucralfate or Losec
•Heartburn – eased by high dose Proton Pump inhibitor (Losec/Prilosec 40 mg bd)
•Volume reflux symptoms persist – regurgitation, waterbrash.
Past History
•RIGHT thoracotomy and repair of congenital TOF in first 24 hours of life.
•Upper midline laparotomy and Nissen-type antireflux fundoplication at age 16.
Repeat bronchoscopy
•Some increase in secretions but not as bad as one might expect.
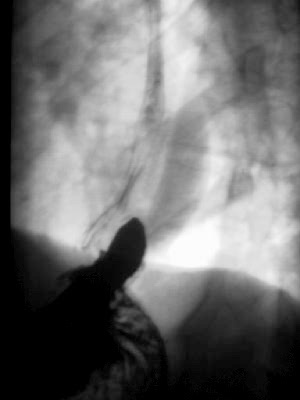
•Fistula visible at base of carina (carina slightly wide with fistula visible at posterior point of carina at its junction with membranous trachea)

•contrast seen in left bronchial tree after first swallow but
•exact position of fistula not demonstrated.
•mixed hernia recurrence noted
•free reflux of gastric contents.
Oesophago-gastroduodenoscopy
•Fistula at 28cm with band of mild stricture (dilated to 60 Fr without difficulty
•Mild oesophagitis (reduced completely by Losec on subsequent OGD), no Barrett’s
•Free reflux of bile and gastric contents.
•Recurrent hernia with sliding and para-oesophageal components.
•Mild chemical gastritis (no helicobacter) and bile +++
•Duodenum normal.
pH study
•Normal daytime reflux (Probe removed by patient during the night).
•De Meester score 3.9 (N<14)
•Good symptom correlation for heartburn (1 out of 2 episodes) and regurgitation (1 out of 1) with acid reflux (>1.5 pH units but not < pH 4)

•Some mild basal inflammation.
•Carina lies one full rib space (the length of one vertebral body) below the inferior wall of the aortic arch.
Current Problems:
1.Recurrent/persistent congenital tracheo-oesophageal fistula – symptomatic and soiling bronchial tree
2.Recurrent mixed sliding/para-oesophageal hiatal hernia – persistently symptomatic despite high dose PPI due to bile reflux and volume reflux. Risk of developing Barrett’s. Para-oesophageal hernia requires treatment to prevent torsion.
3.Bile gastritis – probably not severe enough to warrant surgical treatment.
Options
1.Do nothing – not an option as there is soiling of the lungs and the danger of chronic respiratory disease and bronchiectasis. Also the risk of Barrett's and other sequelae of reflux disease. Para-oesophageal hernia may undergo torsion – (it is already causing crampy intermittent pain)
2.Treat hernia conservatively (see option 1) and re-explore right chest. This is the most direct approach to the carina but it is a previous operative site increasing the difficulty of dissection. Also it seems that the previous right thoracotomy has compromised the serratus and latissimus muscles which I would like to use to separate the oesophagus and trachea. It would be possible to use an intercostal muscle flap but I believe that if I am going to do this at all I intend to do it properly and intercostal muscle flaps are too unreliable.
3.Similar right sided approach associated with laparotomy. It would also be possible to use omentum harvested at laparotomy and passed substernally to bolster the tracheal repair. Via the laparotomy it would also be theoretically possible to repair the hernia. I prefer to do redo hernia repairs (well those done properly via laparotomy as opposed to Mickey Mouse laparoscopic repairs) and virtually all para-oesophageal repairs via the left chest. The previous laparotomy and adhesions are even more reason to use a left thoracotomy.
4.Left thoracotomy (with the option of abdominal extension if necessary to repair diaphragm), harvesting fresh latissimus dorsi from the iliac crest and leaving serratus for any subsequent procedure. Though he is a physical labourer, he is right handed and does not rely on latissimus function as much as serratus. As the carina is seen on chest radiograph to be at least 1 rib space/one vertebral length below the aortic arch it should be possible to dissect this area from the left. We frequently dissect tumours from this position via a left 6th intercostal space thoraco-abdominal incision. After division and suture of the fistulous track the latissimus would be sutured between the two organs to prevent recurrence. The left thoracotomy would allow standard access to the recurrent hiatal hernia (I use a modified De Meester buttressed Nissen-type repair fixed below the diaphragm with "Belsey-type" sutures – known at the Mayo Clinic as "Jonsrud" sutures). The beauty of this approach is the single incision, the virgin pleural cavity and the availability of undamaged muscle. The potential disadvantage is the access to the carina from the left. In this man we would seem to have enough distance below the aortic arch, which can be mobilised further if necessary. We also have experience with tumours in this site and of course routine subcarinal node dissection is easily possible through this approach. The potential adhesion of the azygous vein to the previous TOF repair should not be a problem as full mobilisation may not be necessary and the azygous was probably divided at the previous operation.
5.The ultimate fall-back position would be to perform a total thoracic oesophagectomy via left thoracoabdominal and left cervical (see: Total thoracic esophagectomy for esophageal cancer. Anikin VA, McManus KG, Graham AN, McGuigan JA. J Am Coll Surg. 1997 Dec 1; 185(6): 525-529.) using the well vascularised stomach to patch the back of the tracheal repair (or a three stage with right thoracotomy but it would not be possible to use the stomach as a tracheal buttress.)
Operation
Incision:
•left posterolateral thoracotomy with
•two intercostal incisions - 4th ICS for access to the carina and 8th ICS for access to the hernia
•latissimus dorsi muscle flap raised off iliac crest maintaining proximal blood supply
Findings:
•narrow fistula at level of carina
•surrounding inflammation,
•adhesions from previous surgery and
•lymphadenopathy
•mixed hiatal hernia recurrence
•fundoplication had slipped to "hourglass" the stomach
Procedure
•fistula divided and oversewn
•latissimus brought through a window created by excising a segment of the second rib and placed between the trachea and the oesophagus to prevent further fistula formation.
•hernia dissected and previous wrap taken down
•360 degree 2cm, Nissen-type fundoplication fashioned using o Silk mattress sutures buttressed with Teflon strips. Able to pass one finger easily through wrap. (No bougie passed because of fistula repair above.)
•crura approximated with three sutures posterior to oesophagus.
•wrap fixed to underside of diaphragm using three "Belsey" sutures.
Progress

•Ventilated for three days in intensive careecause CXR showed "left upper lobe consolidation". This shadow is actually the muscle flap which is not seen on the later CXR films.
•Extubated day 3 and minitracheostomy inserted.
•Commenced liquid diet day 5.
•Discharged on liquidised diet day 8 postop.
Re-admission
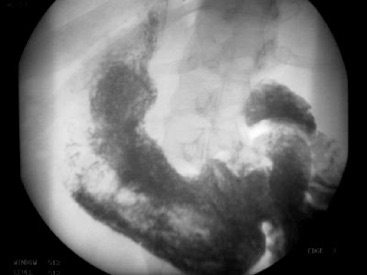
•Re-admitted on two occasions with delayed gastric emptying. Contrast upper GI series confirmed some delayed emptying but confirmed no physical obstruction (Presumably the vagi have been damaged during the four procedures on the oesophagus!) Symptoms gradually abated despite prokinetic agents (Maxolon, Erythromicin)
Review at 6 months

•Returned to work farming
•Off all medication
•Significant weight gain
•Able to eat all types of food.
•Occasional gastric bloating
•Occasional regurgitation of undigested food if he eats to fast - probably being held up above wrap
•No reflux symptoms
•Much fewer chest infections and no hospital admissions.
•Returned to smoking despite advice

