Right sided empyema - left sided thoracotomy!

36 year old girl, severely educationally subnormal with severe kyphoscoliosis presented with a history of being "vaguely unwell for 4 days" with a temperature of 39.7 0C.

The initial chest radiograph was difficult to interpret because of the kyphoscolosis though the radiologist reported definite consolidation of the lower half of the right lung.

Similarly, the abdominal film was difficult to interpret but did show distended loops of small bowel and stomach. The colon was loaded with faeces but she did pass two bowel motions in the fiorst 24 hours after admission.
Surgical emphysema
4 days laterthere was little improvement but an increase in abdominal distension.The general surgical resident was called and found a tense abdomen which was resonant but with occasional bowel sounds. The right chest was dull to percussion.
He requested further chest Xray which showed little change except for the presence of surgical emphysema in the neck,


which is better seen in the closeup (left). Air is also evident within the mediastinum around the heart (right). Though not visible on the CXR he suspected a pneumothorax, ?upper GIT perforation. The patient, whose respiratory function was deteriorating, was transferred to ICU for ventilatory support. A right chest drain was inserted with short-lived improvement.
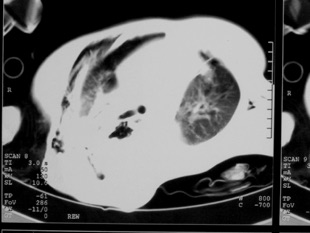
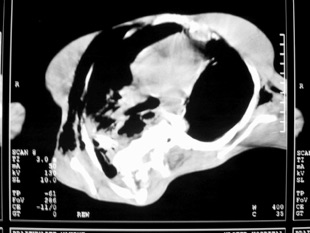
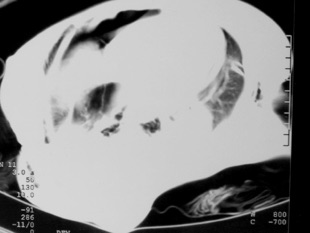
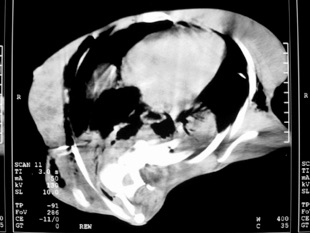
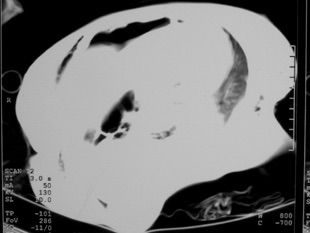
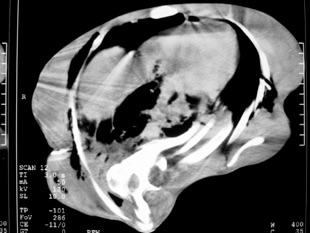
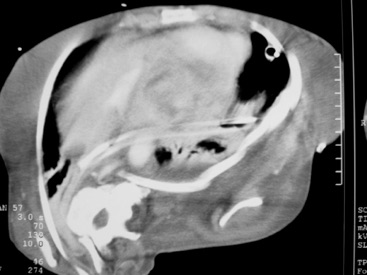
CT scans were requested. They were again difficult to interpret but did show RIGHT sided consolidation and pleural collections with loculations of air and fluid in the mediastinum.
The relevant scans are presented with lung settings to the left and mediastinal windows to the right.
A working diagnosis of perforated oesophagus was made. There were major discussions with the family at this stage. Prior to this episode the patient had, despite her physical disability, led her own life, attending a special school and being very much part of her family circle. Despite the high risk of mortality a decision was made to proceed to surgery.
Surgery: After resuscitation she was taken to theatre and a left thoraco-abdominal incision was made. The logic for the incision was that, despite the right sided changes, the working diagnosis was perforation of the upper GIT tract, possibly related to the previous hernia repair (the globular, air filled shadow in the lower mediastinum was suggestive of a recurrent para-oesophageal sac), and the lower oesophagus and the hiatus are best approached from the left. A thoraco-abdominal incision would give access to the hiatus above and below the diaphragm and access to the abdomen for defunctioning stomas. In addition, a right thoracotomy was not possible because of the body configuration.
Only a single lumen ETT was possible so the left lung remained inflated. Exploration of the left pleural cavity was virtually normal with no free fluid and a normal lung. Only after dissection of the mediastinum was it possible to enter a purulent cavity which extended into the right pleura. In the midst there was necrotic fundus of the stomach which had herniated alongside the previous fundoplication. The previous fundoplication and repair were taken down to reveal that most of the stomach was viable except for the necrotic fundus. The necrotic area was excised with a stapler, oversewn and covered with local omentum. No fundoplication was performed but the crura were apposed snuggly against the oesophagus. A draining gastrostomy and a feeding (Witzel) jejunostomy were fashioned. drains were placed across the mediastinum into the right pleura with routine left chest drains.
The postoperative ICU course was stormy as one would expect when treating an upper GIT perforation of at least 4 days standing.
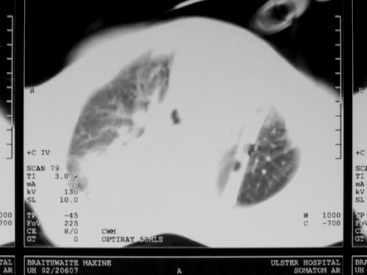
A percutaneous tracheostomy was performed on postoperative day 2 as it could be predicted that prolonged assisted ventilation and airway toilet would be required. There was persistent low-grade sepsis though no specific collection could be seen on a postoperative CT scan. The right apex was well expanded despite no apical drain. A drain placed at left thoacotomy is seen to traverse the mediastinum to drain the right base. There was some residual mediastinal thickening and bibasal lung consolidation.
After a slow convalescence the patient was discharged home to the care of her mother. At six month followup she was reported to have returned to heer pre-illness functional state and was "eating even better than before"!
Final Diagnosis
•Torsion of para-oesophageal recurrence of hiatal hernia
•Perforation
•Empyema
•Mediastinitis
Messages
•40% of hiatal hernia repairs fail by ten years.
•Para-oesophageal hernias do undergo torsion (up to 25% in some series) and should be repaired if the patient is fit for surgery.
•Left thoracotomy gives good access to the lower oesophagus and is virtually obligatory if any reparative procedure is envisaged around the hiatus,even if much of the hernia, and in this case, the empyema are on the right.
