Analgesia Policy for thoracotomy, VATS or chest trauma

Principles
-
•Thoracotomy is one of the most painful incisions a surgeon can make.
-
•Upper midline laparotomy causes as much respiratory depression as a thoracotomy.
-
•All patients who have had thoracotomy, VATS, rib or sternal fracture or even those who have chest drains can be anticipated to have chest pain. It is better to prevent pain than to try to treat it. Therefore pain relief should be prescribed on a regular basis rather than “PRN” or “as required”.
-
•Anticipate pain - give pain relief before physio, drain removal, transfering in and out of bed.
-
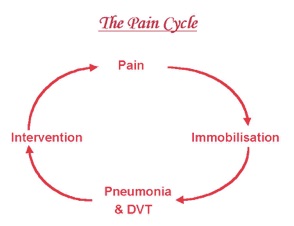
•This pain will interfere with their ability to breathe and their ability to mobilise. Poor pain control leads to increased morbidity for the patient and more work for the doctor!
Standard of analgesia
The standard of analgesia in post thoracic surgery pain is that the patient should be able to move around, cough and work with the physiotherapists and nurses. The standard of analgesia is NOT lying stationary in bed like a beached whale!
There are a number of approaches to analgesia:
-
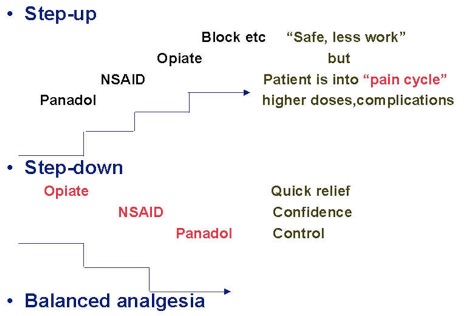
•Step up - this is the traditional way doctors treat most things, trying to get away with as little as possible. Postoperatively this is a recipe for complications
-
•Step down - a better way to get analgesia under control quickly and avoid pain-related morbidity. It can result in overcompensating with narcotics causing its own problems
-
•Balanced analgesia - a modification of step down which uses local blocks and non-narcotic analgesia to reduce the narcotic requirement.
One should anticipate the level of pain and prescribe appropriate regular balanced analgesia comprising of:
-
•Regional analgesia (epidural, paravertebral, intercostal block, local anaesthetic etc.)
-
•Narcotic (PCA or oral)
-
•NSAID +/- Paracetamol (IV, IMI or oral)
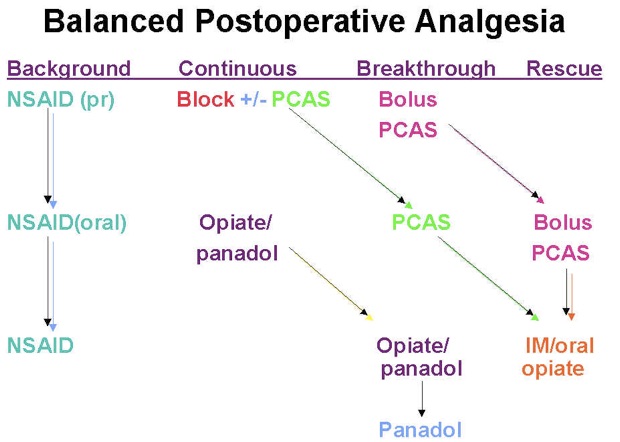
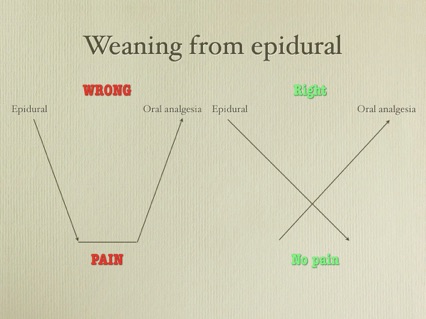
As the pain decreases over the postoperative days, the strength of the analgesia can be reduced. Invasive methods (epidural, paravertebral, PCAS) removed and replaced with oral opiate (Oxycontin, Tramadol). Later these can be weaned to Paracetamol/Codeine (remember to stop paracetamol when prescribing these combined analgesics).
The only time one should prescribe “as required” analgesia is to allow for rescue analgesia (e.g. Oxynorm or opiate imi) . Such rescue analgesia is appropriate when the patient has had physiotherapy, been taken to x-ray or some other intervention which has resulted in greater than the anticipated pain. If the rescue analgesia has been charted to often, this is an indication to increase the regular analgesia.
Weaning from an epidural