Continous Paravertebral Analgesic Infusion

Paravertebral block or "extrapleural analgesia" is a continuous infusion of local anaesthetic over the intercostal nerves as they exit the vertebral column. It can be used after thoracotomy or thoracoscopy. It is almost a unilateral epidural but does not have the same hypotensive side effects. Therefore it is easier to manage postoperative fluid balance without the need for inotropes.
As we make no claims that it is the be-all and end-all of analgesia it is used in conjunction with PCAS and other modalities. It thus avoids the problem of shoulder-tip pain.
It has the further advantage that it is cheap and takes only five minutes to place. Placement is by the surgeon and he only has himself to blame if it takes too long, is in the wrong place, doesn't work, or falls out!
Comparison of the extra-pleural versus PCA performed in our hospital and published 1995 confirmed that superiority over PCA alone (Pain relief for thoracotomy. Comparison of morphine requirements using an extrapleural infusion of bupivacaine. Carrabine U. et al. Reg Anesth. 1995 Sep-Oct;20(5):412-7).
Every randomised trial of paravertebral block verses epidural has demonstrated superiority of the paravertebral block. The technique was popularised in the UK by by Sabaratnam Sabanathan and Allen Mearns in Bradford. Their prospective randomised trial of preoperative and continuous balanced epidural or paravertebral bupivicaine examined post-thoracotomy pain, pulmonary function and stress end points. The paravertebral group had lower pain scores at rest and on coughing, higher oxygen saturations, less respiratory morbidity and lower glucose and cortisol stress responses. In addition there was less nausea, vomiting and hypertension. This would compare with our own findings and clinical practice, and would recommend consideration of this technique for reduced cost and kind implications.
Insertion using Pin buster kit
The On-Q Pain buster is a commercially available device which can be used at open or VATS procedures to deliver a paravertebral infusion.
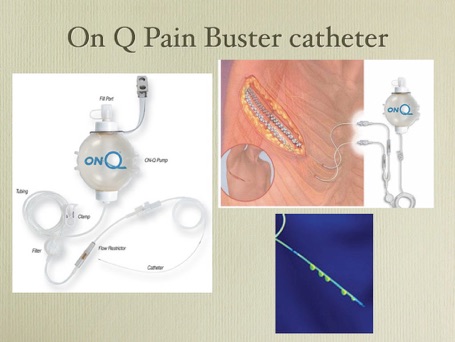
It has tunnelling devices, a soaker catheter, Luer lock and an elastic bladder which delivers a constant delivery rate without the need for pumps, electricity or batteries.
-
•A stab incision (5mm) is made in the skin, 8th intercostal space mid scapular line.
-
•A tunnel is started using an artery forceps, over a rib to the extrapleural space.
-
•The tunneling device with catheter sheath are then bent into a gentle curve and introduced into the extrapleural space.
-
•A tunnel is fashioned back towards the vertebrae and towards the apex. If it closely follows the sympathetic chain, a ready-made extrapleural tunnel often already exists. Once the sheath has been placed high enough to block all incisions, the introducer is withdrawn and the extrapleural catheter inserted into the sheath.
-
•The sheath is then split and removed.
-
•The catheter is sutured to the skin in a loop and the infusion may commence.
Alternative insertion using non commercial equipment
The cheap RVH cannulation technique requires 1/8" Redivac and trocar, anti-bacterial filter, Grey Abbocath and sheath, 20ml syringe with Luer lock, 20ml 0.25% Chirocaine (or Marcaine), 2/0 Vicryl, 4/0 Prolene, 0 Silk on skin cutter.
-
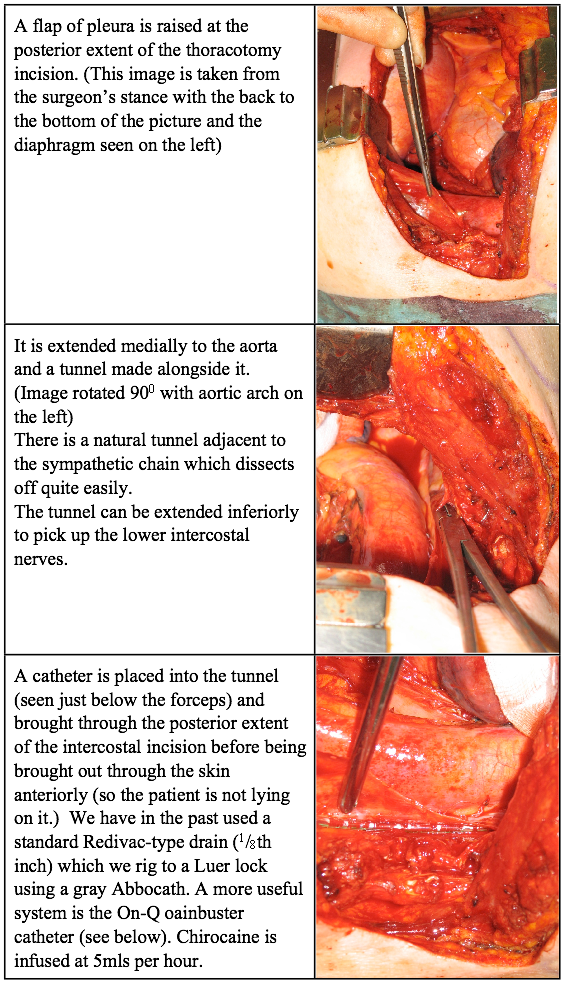
•Starting from the posterior end of the thoracotomy incision, the pleura is lifted off the chest wall making sure it is kept intact. The dissection is extended posteriorly to the level of the sympathetic chain. Superiorly a tunnel is made alongside the sympathetic chain as far up as the stellate ganglion. Inferiorly a pocket is made below the level of the thoracotomy.
-
•An 1/8" Redivac type cannula is lain in the tunnel and contiguous pocket so that the row of holes in the cannula alongside the sympathetic chain, overlying the intercostal nerves as they cross the necks of the ribs.
-
•The other end of the cannula is looped round the divided posterior end of the rib (or brought out through the interspace below the incision), passed deep to serratus, and brought out through the skin in the anterior axillary line (avoiding the drain sites).
-
•Tack the pleura over the cannula to keep it in place with 2/0 Vicryl. If the cannula gets in the way of the thoracotomy closure tack it to the ribs with 4/0 Prolene.
-
•After cutting off the introducer a grey Abbocath is guided into the cannula and sewn in place to give a Luer lock attachment.
-
•To fix the Abbocath I recommend taking the Abbocath sheath and cutting it in half and placing it over the redivac for later suturing. Cut the Abbocath to half its length. Insert the Abbocath (to the hilt) as if the cannula was a vein. Withdraw the needle. Bring the sheath back up to cover the neck of the Abbocath. Place silk suture through the sheath and tie around the hub of the Abbocath)
-
•An epidural type antibacterial filter is connected (the anaesthetists expect it) and the first bolus of 20ml of 0.25% Chirocaine injected.
-
•Thereafter the cannula is connected to an infusion pump injecting 5ml per hour of 0.25% Chirocaine.
The infusion is usually continued till the drains are removed but may be kept longer if required.
Continuous wound infusion with local anaesthetic is also possible using the On-Q Pain Buster system.
