Phrenic nerve infiltration for the prevention of shoulder tip pain

Our anaesthetic colleagues brought to our attention the paper from Liverpool (Scawn 2001) which reported a reduction in shoulder tip pain using lidocaine infiltrated around the phrenic nerve into the cardio-phrenic fat pad. In this study, patients undergoing thoracotomy with epidural analgesia were randomised to receive either lidocaine (10ml 1%) or saline injection into the phrenic fat pad. It seems that shoulder pain was reported in only 33% of the lidocaine patients compared to 85% of patients in the saline group (p< 0.008). Overall pain scores were also lower with lidocaine (p< 0.05). One might expect hypoventilation to result in elevated PaCO2 levels but these were not significantly higher in the study.
The technique I use for phrenic nerve injection is as follows.:

I suspect that some of the pain is actually due to traction and handling of the phrenic nerve during the hilar dissection, as we frequently do not touch the diaphragm or the phrenic nerve below this level but still get shoulder tip pain. The injection should preferably be made prior to the intrathoracic procedure, immediately following the thoractomy incision.
We have found that the phrenic nerve injection is less effective when actually operating on the diaphragm for hiatal or diaphragmatic hernia repair. Contra-lateral shoulder tip pain has been a problem in some of these cases. This would suggest that some of the pain is due to handling of the contra-lateral crus during hiatal hernia surgery. Alternatively, there may be some over lapping of sensory fibres on the under side of the diaphragm which are subsequent transmitted through the controlateral phrenic nerve.
In our own audit of 54 patients undergoing thoracotomy with thoracic epidural, we recorded the interventions required to maintain a pain level of A or B (A - no pain, B - mild pain, C - moderate and D - severe). Interventions included the addition of a non steroidal, the addition of Paracetamol, the injection of the boluses of narcotic, or an increase in the rate of the epidural. We excluded patients undergoing thoracolaparotomy, other incisions of the diaphragm, median sternotomy, staging anterior thoracotomy, chest wall resection and thoracoscopic procedures.
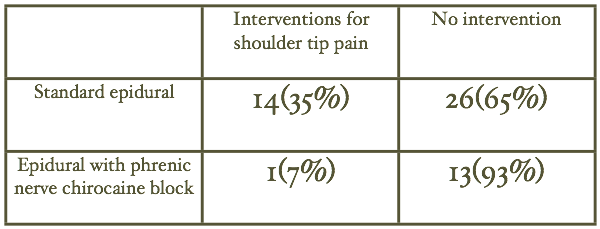
Of those patients who did not have a phrenic nerve block 35% required an intervention for ipsilateral shoulder tip pain. This compared to only one patient (7%) of those who had phrenic nerve Chirocaine block (p = 0.042). The one patient who did require an intervention had long-standing rheumatoid arthritis with extensive pain in many joints and her back. It is quite probable that the interventions were not for standard phrenic nerve mediated shoulder tip pain.
