Clerking Patients


The clerk-in procedure is meant to be an independent overall assessment of a patient’s condition at the time of admission. While it is good training for a trainee doctor, it is also an important safeguard. It is often the case that the patient’s condition has progressed or other co-morbidities have become apparent. The consultant or registrar at the outpatient clinic may have missed important findings, particularly outside his speciality.
If you do find something out of the ordinary, bring it to the attention of the senior medical staff.
Clerk-in for thoracic surgery follows the standard practice, but extra attention is made to performance status and co-morbidities.
Care Pathway
All Thoracic patients, no matter to which ward of the RVH they are admitted, are to be clerked in on the standard Thoracic Care Pathway proforma.
Before you start find …
•Notes
•Xrays including relevant CT's, PET scans and Barium studies, reports and films. Many are now on disc or may have been emailed etc. We require the films to be available for the preop ward round and in the operating theatre as we may need to assess operative subtleties not on the reports. However, it is not only a professional courtesy to take note of the official report, but the radiologist may have seen features on the work station which may not have transferred to the images printed off.
•Referral note - someone has seen the patient before you and has written either:
-
✴GP or referring consultant letter
-
✴Consultant’s outpatient note - this is most important as the consultant will take more attention of his own notes than anything else!
-
✴MDM note (look up on computer)
-
✴A&E note
-
✴Hospital transfer note
-
✴Ward diary entry
Demographics
Name
Number
Date of Birth
Consultant under whom the patient has been admitted – this will determine which particular operating list the patient will be on, which secretary will have the notes and which registrar probably knows the patient. While the consultants try to coordinate protocols as much as possible, there are variations in management and knowing the consultant will have a significant bearing on the direction of treatment.
Date - Today’s date may be the most useful thing you write!
History
Age, Gender, Occupation, referred by...
It is traditional to start with a sentence like: “Mr XXX YYY is 66yr old retired farmer referred by Dr Finlay”. There is good reason for this as it sums up the patient in a nutshell and gives a clue to his condition. A patient’s occupation says a lot about their lifestyle, exposures to toxins and carcinogens and their level of understanding of their condition.
If retired, do not just write “retired” – write retired farmer, teacher, etc.
Note: Including a ‘trigger phrase’ e.g. ‘breeds Abyssinian goats’, will be a stronger hint to your memory than the patient’s name. After a while you will notice that many people have similar names and I would advise caution jumping to a quick conclusion about a patient based on his name only. Pick something unique about the patient. The trigger phrase will bring back the history, the examination, the Xrays and important features of his progress.
Presenting complaint
This is what he wants you to fix so make sure it is recorded. We may be addressing something found incidentally but the presenting complaint will be the patient’s major concern.
History of presenting complaint
Include investigations so far.
Past medical history (including previous operations)
Family History
Social History
Medication
Some people forget to mention inhalers, patches etc as medication.
Allergies
Describe allergies so we know how serious they were. Was there just some nausea and diarrhoea or was there a florrid rash, facial swelling and breathlessness.
Systemic review
•Cardiovascular
•Respiratory (I tend to include smoking history here)
•Gastrointestinal
•Genitourinary/Gynaecological
•Neurological
•Locomotor
Smoking history
Smoking history has a major bearing on postoperative respiratory complications. Many patients will be proud that they have given up and will declare they are non smokers even if their last cigarette was on the day before they were admitted. Get an honest answer without being too accusing. Secretion production increases in the first 3-6 weeks after smoking cessation. Extra secretion management techniques are indicated if still smoking within 6 months of surgery.
Record:
•pack years
•current (i.e within last 6/52) or ex,
•when they gave up,
•pipes, cigars etc
Exercise tolerance/performance status
This is very important in assessing fitness for thoracotomy . It is important to know what the patient is capable of now, not 6 months ago. Some people will tell you they have no dyspnoea on exertion when their only exertion is from the front door to the car!
•On the flat
•On stairs or hills
Performance status is also vital in assessing the ability to tolerate radical radiotherapy and the toxic chemotherapy required for lung and oesophago-gastric cancers though the oncologists tend to use the ECOG scores. In fact, the prognosis for lung cancer correlates as much with performance status as with the disease stage.
Examination
•General
•Hands
•Face
•Neck
•Cardiorespiratory
•Breasts
•Abdominal
It is usually more convenient to inspect, palpate, percuss and auscultate the chest from the front +/- examine the abdomen before sitting them forward to examine the back of the chest
•Gynae (if indicated)
•Vascular
•CNS (and peripheral nervous system)
•Urinalysis
Summary
A three line summary will help you and your colleagues recall who the patient is through the fog of the post-take ward round. For example:
“66 yr old ex-farmer referred from Mid Ulster hospital with 6 week history of haemoptysis. CXR shows right hilar lesion, admitted for bronchoscopy. Past history of AMI x 2.”
Working diagnosis
It is the law of the land in many parts of Europe and other third world countries that a working diagnosis has to be recorded within hours of the patient being admitted to hospital. For some reason Queen's University Belfast graduates have a complete allergy to ever writing a diagnosis. The ability and responsibility to come to a diagnosis is what differentiates you as a doctor from the physician’s assistant who can do everything up to this point. It is why you are paid so handsomely!
Differential diagnosis
The symptoms and signs may be explainable by a number of diagnoses – not all of which may have been evident to the consultant or registrar who saw the patient in the clinic. Consideration of the differential diagnosis will suggest further relevant investigations.
1.Lung tumour
2.Pneumonia with haemoptysis due to Plavix
3.Pulmonary tuberculosis
4.Lung abscess
5.Pulmonary aspergillosis
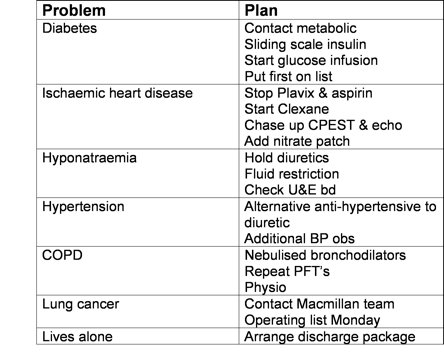
Plan
Your plan will stem from the differential diagnoses which you have completed above. The plan does not just mean a list of routine investigations (FBP, U&E etc) It should give an indication of what is planned for the patient e.g.
•Workup for oesophagectomy
•Anaesthetic assessment
•On list for gastroscopy Wednesday
•Laparoscopic staging Thursday
•Chase up PET scan & EUS result
•Discuss at GIT MDM Friday
If you are not clear of the plan it is imperative, and medico-legally wise to ask the registrar or consultant.
Problem list
Most of our patients, being elderly smokers, have multiple co-morbidities which may have more relevance and cause us more problems than the primary diagnosis with which they have been admitted. It is useful therefore to construct a problem list in addition to the differential diagnoses with a plan for each problem